Diane’s farewell message
After 52 years at WAMU, Diane Rehm says goodbye.
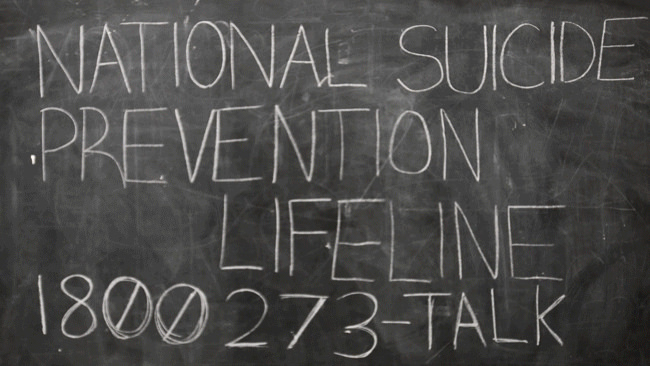
Suicide is the 10th-leading cause of death in the United States. And the suicide rate has grown slightly over the past decade. But a group of psychiatrists and health care professionals is working to change this trend. They’ve launched an initiative that aims to reduce the number of suicides to zero. It sounds impossible, but a health system in Michigan is reporting impressive results. After overhauling the way it screens and treats patients, it reduced the number of suicides by 80 percent. And one year, no suicides were reported. Now others are trying to replicate this success. Diane and a panel of guests discuss the “Zero Suicide” initiative.
MS. DIANE REHMThanks for joining us. I'm Diane Rehm. An effort to completely change how hospitals and clinics screen and treat patients for suicide is underway around the country. With me in the studio to talk about what suicide prevention strategies seem to work and why, Julie Goldstein Grumet at the Suicide Prevention Resource Center and David Jobes with Catholic University.
MS. DIANE REHMJoining us from WDET in Detroit, Brian Ahmedani with the Henry Ford Health System. I do welcome you to be part of the program. Give us a call at 800-433-8850. Send us your email to drshow@wamu.org. Follow us on Facebook or Twitter. And thank you all for being with us.
MS. JULIE GOLDSTEIN GRUMETThank you for having us.
MR. DAVID JOBESThank you.
MR. BRIAN AHMEDANIThank you very much.
REHMAnd Julie Goldstein Grumet, let me start with you. Explain what you mean by the term zero suicide.
GRUMETIt's really an aspirational goal. There is no other number that you could fill in and say we'd be comfortable if our organization had ten suicides, right? Who are those ten people? It's an ambitious goal, but it's aspirational that a healthcare system should be striving to reduce their suicides down to zero, constantly improving their practices, their performance, their data collection, their policies, their training to get to zero.
REHMDo we know how many suicides occur each year?
GRUMETThe most recent data from the CDC is from 2013 and it was about 41,000 suicides in the United States and it's the tenth leading cause of death.
REHMAnd to you, David Jobes, how do you see this project zero? Is it different? Is the approach different from anything we've done in the past?
JOBESIt's a complete game changer, Diane. I've been working the field suicide prevention for 30 years and there's never been before a time like now where this initiative has really taken root and is causing significant changes in how we think of the care at the systems level and also at the clinical level in terms of preventing and saving lives.
REHMAnd to you, Brian Ahmedani of the Henry Ford Health System in Michigan, I know was very successful in reducing suicides by how much?
AHMEDANIWell, the zero suicide initiative, it's called Perfect Depression Care here at Henry Ford and the original rate of suicide in our population was about 100 per 100,000. And this is for our behavioral healthcare patients. The rate now is around 20 per 100,000 less than that since the initiative started.
REHMAnd can you explain as little about the program and what it entailed?
AHMEDANIYeah. So basically in the same concept of what the Zero Suicide Initiative is nationally, this is a comprehensive approach. It's a model that specifically got designed to reduce suicide in our behavioral health population by incorporating several different components into clinical care. So we have several different risk stratification models. We focus on lethal means restriction or weapons protocols, suicide risk assessment, continuous learning.
AHMEDANIAnd I think the most important thing, if you talk to Ed Coffey, who is the person who originated this program, the most important thing for him has been that there is a just culture, meaning that everyone feels okay about talking about these types of things. If there is an error, we can work on it and fix it. And then, the other thing is that everyone is committed to zero suicides, meaning that every single person knows about the program and they're committed to working towards achieving that zero goal.
REHMAnd Julie, I gather that means you don't give up on a patient.
GRUMETAbsolutely. That's correct, Diane. I think the idea is that you must screen everybody who enters your doors to know whether or not they're at risk for suicide.
REHMHow do you do that?
GRUMETThere are standardized screening and assessment tools that organizations can use.
REHMGive me an example.
GRUMETThere are those that are in the public domain, one is called the Patient Health Questionnaire 9, PHQ9. It's nine questions. The ninth question references suicidal thoughts and it can easily be administered. And for those who say, yes, you want to know what is their degree of risk and you can do a risk assessment. Again, you could do standardized risk assessment tools because people's training varies so greatly that not all clinicians are well prepared to do a good risk assessment.
GRUMETAdditionally, sometimes people have biases and say, I know him or her. She would never take her own life. And so they really kind of weed out people in their own mind who they think may or may not be at risk and they don't assess for risk. And we know that you have to screen and assess everybody who walks through your doors.
REHMDavid Jobes, as a clinical psychologist, can you help me to understand the kinds of questions you might use on a one to one basis, not so much on paper, but in talking with a patient or a client that might give you a hint that that person has thoughts of suicide?
JOBESSure, Diane. We think about asking and talking about suicide very directly. You know, have you had suicidal thoughts? In the mind's eye of a suicidal person, this is a conclusion that they may come to that this is a way that they can get their needs met. And so when we ask very directly about it, we're going to ask more questions about hopelessness or questions about their self esteem or their psychological pain and to have a very open conversation about it is actually very soothing for the patient.
JOBESIt's a very difficult topic to talk about, even for mental health professionals.
REHMCan you always get that person to admit that he or she might be having suicidal thoughts?
JOBESNot always, but typically if people bring themselves into care, they're, at some level, interested in being asked and being engaged with. We find in the intervention developed in my group that we literally sit next to them and go through an assessment tool together to engage them in a discussion about the struggles that they're going through in which leads them to think that suicide's the way I deal with my situation.
REHMSo Brian, once a patient or a client is considered someone who's at risk, what do you do then?
AHMEDANIYeah, sure. So that's a great question. I mean, and actually the interesting part of our program at Henry Ford is that everyone is considered to be at risk who's in behavioral health. And that's mostly just because the national rates suggest that, you know, people with mental health conditions have an increased risk for suicide. So for us, it's everyone is considered to be at risk. And then, after that, there's a set of protocols that are in place and so, you know, we have specific care pathways depending on how much we consider the risk level of that person.
AHMEDANISo people are either at immediate risk or have a lower level of risk. And depending on that level, it triggers a care pathway as to what someone needs to do clinically. And basically, we have a protocol set up so people have visits within a certain number of days, depending on what level of risk they are.
REHMJulie, can you add to that?
GRUMETYeah. I think the fact that the system has in place these care pathways, both is reassuring for the staff person as well as the patient. The patient should be educated much like anybody even in the medical world would be educated about a recent diagnosis of cancer or diabetes. Here's how we're going to treat it. Here's what our plan is for you. Here's how often I plan to see you. Here's what happens if you don't take your medications. Right? The same thing needs to happen for behavioral health and specifically for suicide.
GRUMETHere's our organization's plan to work with you because you're at risk for suicide. This is what will happen if you don't show up for an appointment. We will need to find out to see if you're safe. We'll come. We'll call you. We'll look to make sure that you're safe.
REHMSo how much of the approach involves medication? How much of the approach involves seeing a patient face to face?
GRUMETIt's a system's based approach. It's a comprehensive approach and so it's not really explicitly about any one medication, any one treatment modality. The idea is that if somebody is at higher risk for suicide, as Brian said, that the system would have in place a management plan. You would do a safety plan with them. You would counsel on their access to lethal means and reducing access. You would provide them with evidence-based treatment when they come into sessions and you'd likely expect to see them at least weekly, if not more, and you'd have a plan in place for when they miss appointments. And part of that management structure may include medication.
REHMAnd David, it would seem to me a system's based approach is very wide, but the individual's need is very narrow.
JOBESIn the system's context, there are very particular individual needs of a suicidal person and they vary. So not all suicidal people look and sound the same and so as Julie eluded, there's different approaches, different evidence-based approaches to treating suicidal risk. And the evidence really shows that targeting suicidal risk as the focus is the way to go.
REHMDavid Jobes, he's professor of psychology at Catholic University and a clinical psychologist. We'll take a short break here. We'll take as many of your calls as we can throughout the hour. Stay with us.
REHMWelcome back. We're talking about suicide prevention and new approaches that seem to be having really a significant effect on reducing the number of suicides in this country. Here in the studio, Julie Goldstein Grumet. She's a clinical psychologist and at the Suicide Prevention Resource Center. We're going to have phone calls up on our website -- phone numbers on our website for those who would like to have assistance. David Jobes is here in the studio. He's professor of psychology at Catholic University and a clinical psychologist. On the line with us from WDET in Detroit, Mich., Brian Ahmedani, director of psychiatry research in the behavioral health service department. He's at the Henry Ford Health System in Michigan. He is an epidemiologist.
REHMWe have an email here from Drew, who says, please address soft suicide in the U.S., people who eat, drug, drink themselves to death, people who are non-compliant patients who continue poor self care, knowing it will kill them. He says, we covered this topic in grad school psych class. It opened my eyes. What do you think, David Jobes?
JOBESWell, there's the notion of a passive suicidal psychological state where you basically just live in such a way that gets you, over the long term, in dire straits. You don't eat well, you know, you drink too much, you drink and drug, that there's sort of a passive, unconscious death wish. One of the big struggles in treatment is getting such people into treatment and getting them motivated to actually seek that care and the treatments that we know that work.
REHMAnd perhaps even to admit to themselves that that is their goal.
JOBESYeah. I think a clever clinician, a skilled clinician, working a proper system of care, can engage somebody around that behavior and raise the question to bring the care that we would like to bring to help save that person's life.
REHMAll right. I'm going to open the phones, 800-433-8850. First, to New London, N.H. Janna, you're on the air.
JANNAHi. Thanks. This is a hard topic, but...
REHMIt sure is.
JANNA...there's a group that I'd like to mention that might not be being addressed, is those who don't see a counselor, that their friends and family who are close to them might see different signs adding up and, if they talked to each other, they might see a risk. This is the person who's not voicing suicide. And if something puts them over the edge among several, you know, overwhelming things in their life, that it's called spontaneous suicide. And this happened to someone in my family recently.
REHMOh, I'm sorry.
JANNASo it does -- thank you -- it's a shock and a horror and a devastating thing. And that's just something that I wanted to say. If there wasn't an active method available, like a gun, then this person might -- they tend to not do it. And then they would get through that very low point.
REHMJulie.
GRUMETWell, I'm so sorry for your loss.
REHMIndeed.
GRUMETI do think that -- we do know that access to lethal means is really the single most concern when people are at risk for suicide. One of the really kind of universal approaches, just even in the community, is the idea that if family members believe somebody may be at risk for suicide, is just removing their access to whatever the lethal means is. And most often, it's a gun because of its high lethality. You know, finding -- there are partnerships even with police stations, there are lockboxes, there are -- just really getting it out of the house, during just the acute crisis. It's not around -- I think we struggle in this country around the relationship to gun control. And this isn't about gun control, it's really somebody's safety.
REHMDavid Jobes, to what extent does the assistance of not only a family member but a friend of the family trying to help this person get to a counselor. To what extent can that make a difference in preventing suicide?
JOBESI think it would make a huge difference. I mean, one of the most awful parts of the suicide challenge is that people are impacted, like the caller, in these awful, terrible ways, and have many regrets, typically, in hindsight. So we, in the suicide prevention community really advocate that if you're concerned for a loved one, you know, reach out to them and try to get them into some professional help, if possible.
REHMAnd perhaps, Brian, go with that individual to see a therapist?
AHMEDANIYeah, absolutely. Sure. I mean, in our program at Henry Ford, we certainly -- that one of the tenets of the program is to involve the family. We bring them in. And they're the, you know, they're key. If the family is not involved, it's much more difficult. Because they're the ones that are there with the people every day. And support is very key to suicide prevention.
REHMAll right. Let's go to Chapel Hill, N.C. Larry, you're on the air.
LARRYHello. Yes. My father went through this ordeal and it -- basically, my whole premise is that you have to talk and communicate. Because I remember, after he had a couple of attempts and they were going to take him -- all our siblings got together and decided whether he has shock treatments or not, I said no. I'm the only sibling that said no. The other three said yes. And as I was taking him -- walking with him -- well, he's on a gurney, you know -- and I walked with him down to the treatment. I said, Dad, you only had a problem with me. You just had to talk to me. You know, that what happened to my son, he was young and the injury that he received, you had a problem with that and you should have just talked to me.
LARRYAnd he said, yes, you're right, Larry. And if I had just talked to you, I wouldn't have -- I won't be -- I wouldn't have been where I'm at today. And really that's -- we've always talked. But then he stopped. Because he did something he thought he shouldn't have done. And I forgave him for it and it's (word?) . And now you just got to talk. And you didn't. And that's one of the most important things to do in any psychosomatic situation is talk.
REHMAbsolutely.
GRUMETYeah. I think it's really, as Dave said, it's when people, loved ones, people in your life suspect that you're struggling with thoughts of suicide, they have to take it seriously, right? We wouldn't ignore symptoms if we thought somebody was having a heart attack. We would take them to the emergency department and help them seek the appropriate medical care. And I think that's not always the same with behavioral health. We sometimes think, if we support the person enough and love them enough, we can love them out of it. And that's not the case. People are struggling with real, significant issues and they need to see skilled and professional providers to deal with it.
REHMI gather that in Zero Suicide, patients have to become a part of devising a strategy to keep them from taking their own lives, Julie.
GRUMETSure, that's called a safety plan. I mean, really it's the idea of what is -- and it's individualized, right? What keeps me safe isn't the same for you.
REHMOkay. But give me a specific set of steps that one does if you're target A.
GRUMETAs part of my treatment, once it's -- once I'm recognized to be at risk for suicide, I should sit collaboratively with my provider and talk about what are my triggers? What are the times that I feel more suicidal? And then what am I going to do when that happens?
REHMWhat might those be?
GRUMETIt may be -- it's things that are coping skills for me. So maybe it's playing with my dog, talking to my husband, if need be, calling my therapist, calling loved ones who have been trained and educated about what to do when they receive that phone call. It's a long list of coping strategies that then I review with my clinician every session to say, did I try it? Did it work? How do we change it to make sure I'm continually using it in an effective way and keeping myself safe?
REHMDavid.
JOBESIn effect, Diane, suicides don't happen out of the blue. And the effective treatments train the patient to recognize how, when, where and why they get in trouble. So they become a suicidologist of sorts of themselves. They learn to recognize that I'm headed in a direction where I may get in trouble. I may be heading into a dark moment. And then the treatments that are evidence based then treat -- then train them to do things instead with tricks of coping, different kinds of problem-solving strategies to address those dark moments and those states that people get into.
REHMBut, perhaps, they don't even recognize those.
JOBESThat's exactly -- that's exactly what the treatment does then, is to help them recognize that this does not come out of the blue and to recognize, when they get in trouble, what to do.
REHMAnd joining us now is Diana Cortez Yanez. She is an advocate for preventing suicide. She has actually, herself, been treated for depression and for being suicidal. Diana, thank you so much for joining us. In your 20s, I gather, you became depressed. Later, you tried to take your own life. You were given antidepressants but that did not work. Tell me about your experience.
MS. DIANA CORTEZ YANEZHello, Diane. And thank you for having me.
REHMCertainly.
YANEZYes. It was, as soon as I started with depression, I immediately was suicidal and I didn't understand it. It -- I was, my culture, we didn't experience a lot or at least didn't speak about suicide. I didn't know anybody who was. So I really felt alone. And I went to a medical doctor, was given these antidepressants. And they didn't seem to be working at the time, they were trying different types. And they just didn't seem to be working. So my suicidality -- it was a matter of thinking about taking my life and not wanting to be around is what basically happened during that time.
REHMHmm. And you're listening to "The Diane Rehm Show." You were hospitalized for a certain period but apparently that didn't help you. Do you know why?
YANEZYes. I went several times to -- I started out with therapists, different therapists. And eventually, there was an attempt, because you go from -- at least I went from suicidal ideation, where I was thinking about it all the time, to planning it and eventually attempting it. So once I was hospitalized, I found that -- my therapist and I had never even discussed suicide. It was never addressed directly. And then once I got into the system, it wasn't approached either -- not by the ER staff or even once I went into the -- I was put into the mental health floor.
YANEZI was also -- they said I was going to see a psychologist. Once I did, I got -- the psychologist just asked about my medication, didn't ask me what the situation was, how it was that I got there -- to the place where I was. He adjusted the medication and that was it. So not any of the needs -- the emotional needs, for sure, were addressed when I was in the hospital.
REHMI see. But I gather things changed for you in 2010. You ended up in a hospital where they used new therapy treatments. What happened then?
YANEZYes. Exactly. After four attempts, and on my fifth attempt, I was in the hospital. I was hopeless from my end. I knew what the -- a routine was. You know, I would go into the hospital for two or three weeks and then just come out to the exact same situation. This time was completely different. The psychologist that I saw immediately just mentioned suicide to me directly, looked me in the eyes and told me he understood where -- that I was suffering and that he had hope. And those words, coming directly -- as the professionals have mentioned already -- were something that immediately gave me an immediate change of looking at my future.
REHMHmm.
YANEZAnd then, after that, I actually entered into an evidence-based therapy, which is called dialectical behavioral therapy and I was in that for a year. And I'm no longer suicidal.
REHMI'm so glad to hear that. What do you want other people to know about your own experiences?
YANEZI think that for families, I would like just to know that even though it seems like a very scary subject, it's very important that it be brought up and be talked about. There are professionals out there -- and especially now, more and more -- even the medical staff, everybody's talking more about suicide. It's important to let them know there's hope, that things can seem dire at the time when they're thinking of this, especially if there's different situations. But there is hope out there and there is professional help and that they're loved and will be helped, you know, during the whole process.
REHMWell, I want to thank you so much for joining us. Diana Cortez Yanez, she's an advocate for suicide prevention strategies. Thanks very much for being with us.
YANEZThank you for having me.
REHMAnd David Jobes, it sounds as though real, one-on-one connection with the doctor, in addition to follow up, can make a big difference.
JOBESYes, Diana has just spoke to it. There's an avoidance. There's avoidance at the family level in our culture and society. There's also avoidance, amazingly, among mental professionals. And so what we're really talking about here today is a very frank, straight-forward engagement in a non-shaming way about this topic, to then implement evidence-based practices.
REHMSo it sounds as though you're saying even the doctors have some reluctance of saying, well, clearly, you are suicidal and I want to help you. I mean, it sounds as though doctors are concerned about that.
JOBESWell, we're human too. It's a -- it is a difficult topic. This whole show is hard to address such a complex, difficult topic. And yet that is the way we save lives is just a very forthright conversation, empathic conversation, to talk about what are your needs and how can we give you hope? Just like Diana stated. That's a big game changer.
REHMDavid Jobes, professor of psychology at Catholic University and a clinical psychologist. We'll get back to the phones after a short break. Stay with us.
REHMWelcome back. We're talking about suicide prevention in a season when suicide may go to a very high level. Here's an email from Jennifer, "Could your panel please comment on early teen suicide and how it differs from adult situations? My son has been anxious and, in my opinion, depressed for a long time. He's met with a couple of counselors over the years, but does not appreciate them prying into his personal life." David Jobes.
JOBESWell, this is a second leading cause of death for 15 to 24 year olds, so we do have a lot of focus on adolescent and youth suicide. And a lot of times young people are reluctant to talk to an older therapist. There's a lot common across the suicidal states. I think what's uncommon in the youthful suicidal mind is a lack of experience, a lack of perspective. They tend not to have much wisdom to draw from.
REHMAnd perhaps even an impetuousness.
JOBESOf course. And then there's also the issue of being depressed invariably involved some distortions in the way that they think. So the challenge is finding a thoughtful therapist that can engage the adolescent mind, and really talk about what's at stake and work with some of those distortions.
REHMDo we know how effective talk can be in dealing with someone, a teen for example, Julie, who says -- or does not even admit he is suicidal?
GRUMETI think the research shows that there are evidence based treatments available, both for youth and for adults, to specifically address the thoughts of suicide. Cognitive behavior therapy, dialectical behavior therapy, the collaborative assessment and management of suicide, which is Dr. Jobes' treatment approach. They have all been researched and they show a reduction in suicidal thoughts and behaviors when used.
REHMBut what about the cost of implementing this whole kind of zero approach to suicide? I gather you, David, have some concerns about that.
JOBESOh, I have a realistic appraisal that, you know, inpatient care can be very expensive. And there's an automatic assumption that inpatient care is the first response. In my view it really should be the last response because these evidence based interventions can be primarily done on an outpatient basis. Inpatient care can absolutely be lifesaving in the most extreme cases, but I think one of the virtues of the zero suicide prevention initiative is that in the long-term it may be actually cost savings.
REHMBut what about if someone does commit suicide on your watch, Julie? I mean, you're taking on a lot of responsibility.
GRUMETHealth care systems are seeing people at risk for suicide regardless. So the zero suicide initiative really is the idea that the system should be more aware, more responsible, and provide a supportive system and framework for their clinicians. They shouldn't assume that because they have licensed professionals working for them, that they know how to treat people at risk for suicide.
GRUMETAnd the zero suicide approach really puts in a safety net that both improves patient safety as well as staff safety. It's not to identify a staff person and say, you had a suicide and so you did something wrong. It's clearly there's a gap in our system that we need to fix. Because if it happened to you, it will probably happen on others' watch as well, and we need to fix and improve it.
REHMIs the title "Zero Suicide" realistic, David?
JOBESSuicide's aspirational. What I would really advocate is best possible care. Because that we can absolutely deliver. We can absolutely do good assessments, thoughtful assessments, stratify risk, and bring evidence based suicide specific treatment to the care of our -- the work that we do with our patients.
REHMAll right. Let's go to Linda on Long Island, N.Y. You're on the air.
LINDAGood morning, Diane.
REHMHi.
LINDAHi. I ask that you just listen to my perspective before commenting. I've been extremely depressed at times. And in other times I've been helpful to those who've been depressed. We all go through ups and downs. We live in a very crazy, upside down world right now. Trust, inclusion, love, those are the things that we need most. We need to feel community. We need to feel the human, not the clinical. We need to feel that our family is everyone, not just the members of, you know, our parents and our siblings who sometimes don't understand. But love is what everybody needs. Recognition to be heard, not to be fixed. Us, we, versus them. No condescending. When we're down, we just need to be affirmed by those who care about us.
REHMJulie.
GRUMETLinda, I couldn't agree with you more, that I think that absolutely love, connectedness, not being judged by your family and your friends, and having a supportive network is incredibly necessary for people who are struggling with anything, especially suicide, but really with any of life's problems. But just like any disorder, there are treatments available, and loved ones should recognize that they need to help you to find a provider and a system that can also be part of your network. You need to have a vast network that includes professionals as well as your family, loved ones, community supports.
REHMHere's an email from Donna, "How do you find out that suicide is on the radar of a loved one and seek help? Most warning signs are only apparent after the fact." Brian.
AHMEDANIYeah, no, this is a really good question. And often we look back at suicide and we think, you know, what should we have known? You know, what is there that we could've done? Often there are some signs. You know, there are people that are changing their behavior patterns. They're doing less or they're doing more of the everyday activities that they start doing, or that they're always doing.
AHMEDANIYou know, what we have to do is really care about your family and our friends. And, you know, sometimes people will speak out. And if you're open, and if you're willing to talk with your family members and friends, then there's no question about it that, you know, often they will bring up these things. You know, and I think we just have to be close. We're not going to get -- they're not going to say everything, but we do have to be open and willing to talk with them.
REHMBut surely Donna has a point, David, that there are some who don't talk about it at all.
JOBESThere are some, but I think the vast majority would if they were so asked. And so simply caring to ask is really critical to saving lives.
REHMAll right. Let's go to Raleigh, N.C. Jennifer, you're on the air.
JENNIFERHi. I just want to thank you and your guests for taking this topic today. And to say that I've learned from a family experience the importance of a couple of things. One of them is the fact that when a person commits suicide, it can have a profound effect on people that goes beyond anywhere that they would imagine. And the second being how important it is for the people who are affected by it to have access to support for processing their feelings. I have an uncle who committed suicide in the early 1940s before I was ever born, and all the members of my family who were alive at that time are no longer alive, but it's still having a profound effect on my family.
JENNIFERWhat happened was, he lived in a small, Midwestern town. He was rejected by his girlfriend. He didn't have much money. He borrowed a little bit of money from my mother. With that money he bought common farm poison and committed suicide. And as you can imagine, in a small Midwestern town, this was headline news. But my mother was afraid that her children would think that somehow this ran in the family, so she never talked about it, including with her children. And she was so fearful about it that when -- just kind of the way she socialized her kids, she just couldn't tolerate my brother having any kind of frustrating experiences, and it didn't serve him well in terms of how it trickled in his life.
JENNIFERIt wasn't so much so with my sister and me. But it's clear to me that even today in terms of where each of us is in life, it's still having a profound effect.
REHMInteresting. Julie.
GRUMETYeah, I think, you know, what we can see with somebody like Diana, who's one of the speakers on the call today, is the idea that if people can begin to tell their stories more, feel more comfortable sharing, that's one of the ways that we're going to really reduce suicide. It can't be something that we whisper about and that nobody understands, because then even within families, when we don't know that there are thoughts of suicide or depression or mental illness, it's hard to great treatment. I think Diana and many others like her who have the experience of suicidal thoughts are able to share their stories and we can learn from them.
REHMAnd you're listening to "The Diane Rehm Show." I think the other important point our caller raised is the profound effect that suicide can have through the generations. David.
JOBESThere's no question that suicide is a uniquely awful way to lose someone. And invariably people feel like there are things they should've or could've done in hindsight, which is why we're advocating so much to ask the question, to reach out if you have concerns.
REHMBut there's also that notion we heard from the mother of a young boy who didn't want to be pried, who didn't want to be backed into a corner. You know, how do you raise such a subject? What are the means by which you can do that without seeming to be prying or threatening? Can you speak to that, Brian?
AHMEDANIYeah, I think in the past, what we've done so much is talk around this subject. We've talked about depression. And we've talked about feeling hopeless and sad. And I think the message here, what David and what Julie are trying to say, is that we actually have to ask the question specifically. And we haven't really done that before. Suicide prevention, suicide treatment has not really existed. It's always been mental health treatment. So now what we're trying to do is shift the way that suicide prevention, you know, how it occurs, and we're actually focusing on suicide almost as a separate condition.
REHMSo you're saying that perhaps a parent, perhaps a friend, a sibling might simply say, you seem to be a bit down, are there thoughts in your mind of ending your life?
GRUMETExactly. We know that people fear doing that because they're afraid they'll put the idea in somebody's head or...
REHMRight.
GRUMET...it will make them mad. And research does absolutely not bear that out. People want to be asked. It's very scary to tell somebody you're having thoughts of suicide, and not know whether you'll be judged. But when somebody asks you in a nonjudgmental, caring way, it opens the door for something that perhaps your loved one has been struggling with and didn't know how to tell you.
REHMAnd here's an email from Julie in Maryland, "Please comment on the use of ECT, electro," something therapy.
JOBESConvulsive therapy. What's commonly not known perhaps for among your listeners is that the treatments that treat suicide effectively are psycho social. They're the treatments that Julie described.
REHMMore than the shock therapies.
JOBESMore than medication and more than electroconvulsive therapy. There are several psychotic depressions where ECT can be effective, but that real treatments are psycho social in nature.
REHMSo you're saying even those doctors who are recommending electroconvulsive therapy know that talk and medication are more effective?
JOBESNot necessarily, Diane. I think there's a pervasive notion that medication and hospitalization is the primary way that we should address suicide risk. My view is that the evidence based interventions that are talk therapies is where the science lies.
REHMAnd here's something to that effect from Scott, "Please address involuntary commitment. I went through this myself this summer for four awful days. And I was not suicidal. Your experts make it sound so scientific, sanitized and caring. But the assessment for hospitals is nothing of the sort. They're just looking to take care of themselves from a liability standpoint. I'm not scared to death of admitting anything for fear of having my rights taken away again." Brian.
AHMEDANIYeah, this is a great question because I think that's really happens when people end up in inpatient. They do, they feel like they're in jail. I mean, this is a terrible situation. As soon as someone tells you that they are having thoughts of wanting to hurt themselves, we lock them up and don't let them have access to anything that they want. It's really a crazy model. And, you know, there's some thought about changing the way that that -- you know, we need to move forward into the future with that. And David touched on that a little bit about different models that actually outpatient treatment may be more effective than just putting someone in an inpatient hospital.
REHMSo your final message, Julie, is what?
GRUMETThere are treatments available to address thoughts of suicide, but you need to have a skilled professional provide it if the symptoms are acute, severe, and if the family doesn't know how to assist the person. Then most people respond well to these treatments, but you need to have a health care system that embraces the person's thoughts of suicide and knows how to manage their suicidality.
REHMAnd David?
JOBESThat there is hope. That there are effective treatments. But it's hard to these effective treatments if we don't ask.
REHMJulie Goldstein Grumet, she's a clinical psychologist. David Jobes, also a clinical psychologist. And Brian Ahmedani, he's at the Henry Ford Health System in Michigan. Thank you all.
JOBESThank you, Diane.
GRUMETThank you.
AHMEDANIThank you.
REHMAnd thanks all for listening. I'm Diane Rehm.
After 52 years at WAMU, Diane Rehm says goodbye.
Diane takes the mic one last time at WAMU. She talks to Susan Page of USA Today about Trump’s first hundred days – and what they say about the next hundred.
Maryland Congressman Jamie Raskin was first elected to the House in 2016, just as Donald Trump ascended to the presidency for the first time. Since then, few Democrats have worked as…
Can the courts act as a check on the Trump administration’s power? CNN chief Supreme Court analyst Joan Biskupic on how the clash over deportations is testing the judiciary.